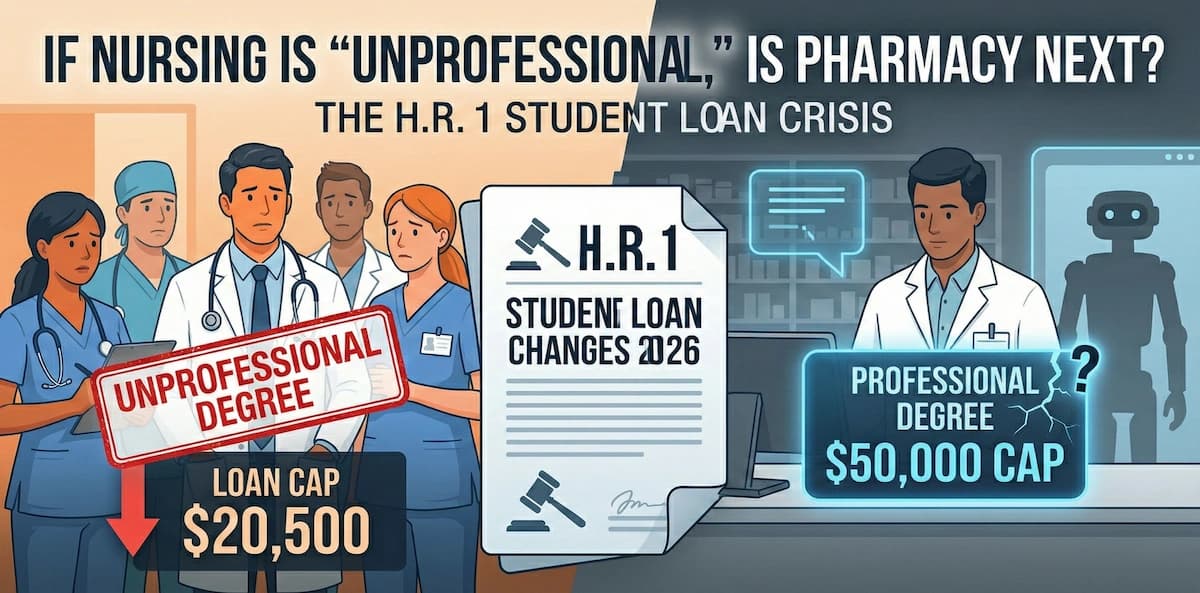
If Nursing is 'Unprofessional,' Is Pharmacy Next? The 2025-2026 H.R. 1 Student Loan Crisis
Disclaimer: This article is for educational purposes only and does not constitute financial or legal advice. Student loan regulations are subject to change; always verify with your financial aid office.
The "Unprofessional" Shock
It wasn't a tweet; it was a PDF dropped on a Friday that fundamentally altered the American healthcare landscape.
For decades, the healthcare hierarchy has been defined by the "Medical Model." Physician Assistants (PAs) built their entire professional identity on this foundation. They train alongside medical students, they rotate in the same residencies, they sit for rigorous boards, and they practice medicine under the same liability frameworks.
In my analysis of the healthcare landscape, I have seen PAs assume that their alignment with the Medical Model was a shield against administrative devaluation. They believed that because they functioned like physicians in the clinic, they would be treated like physicians in the budget.
H.R. 1, the "One Big Beautiful Bill Act," shattered that shield.
When the text of the OBBBA was released, the shock wasn't just that nursing was labeled an "unprofessional degree." It was that Physician Assistants—despite their strict adherence to the medical model—were stripped of professional status alongside them.
Effective July 1, 2026, the federal government is drawing a jagged line in the sand. If you are an MD or DO, the government trusts you with $200,000 in federal leverage to finance your education. If you are a PA or NP performing primary care in the same clinic, managing the same hypertension and diabetes, the government values your education at 50% of your colleagues.
This is not just a budget cut; it is a redefinition of the healthcare team. It signals that the government views Advanced Practice Providers (APPs) not as autonomous professionals, but as technicians who should be trained cheaply or not at all.
What is the H.R. 1 Student Loan Change 2026?
To understand the panic in admissions offices across the country, you have to look at the numbers. The OBBBA splits federal graduate student lending into two distinct tiers based on degree classification, effective July 1, 2026.
Tier 1: "Professional" Degrees
- Status: Protected.
- Annual Cap: $50,000 (Unsubsidized).
- Aggregate Cap: $200,000.
- Degrees: Medical Doctor (MD/DO), Doctor of Pharmacy (PharmD), Doctor of Dental Surgery (DDS/DMD), Doctor of Veterinary Medicine (DVM), Doctor of Chiropractic (DC), Juris Doctor (JD), Clinical Psychology (PhD/PsyD).
Tier 2: "Graduate" Degrees
- Status: Demoted.
- Annual Cap: $20,500 (Unsubsidized).
- Aggregate Cap: $100,000.
- Loans Eliminated: Grad PLUS loans are gone for new borrowers.
- Degrees: Nurse Practitioner (NP), Physician Associate (PA), Certified Registered Nurse Anesthetist (CRNA), Doctor of Physical Therapy (DPT), Occupational Therapy (OT), Masters in Public Health (MPH).
The Department of Education claims this is "not a value judgment" but merely an internal definition to "distinguish among programs that qualify for higher loan limits" to curb tuition inflation.
But let’s be honest about the math. A CRNA program costs upwards of $90,000 in tuition alone. By capping federal loans at $20,500, the government is forcing students to find $70,000+ per year in the private market. This effectively privatizes the cost of education for the providers who make up the backbone of the safety net.

The "Medical Model" Fallacy: Why PAs Were Cut
Why were Physician Assistants excluded from the "Professional" degree list?
This is the question burning up forums on r/physicianassistant. PAs were created in the 1960s to address physician shortages by fast-tracking medical training for combat medics. Their curriculum is modeled on medical school: didactic years followed by clinical rotations.
Despite training on the medical model, PAs were categorized as "non-professional" largely due to cost-cutting measures targeting high-volume degree programs. The Department of Education excluded PAs, NPs, and PTs to rein in "inflated prices," ignoring the clinical reality that these providers function similarly to the physicians and pharmacists who retained Tier 1 status.
The "Chiropractic" Insult
The distinction is arbitrary, yet the financial violence is real. I have reviewed the list of "Professional" degrees protected under Tier 1. Look at it closely:
- Chiropractic (DC) made the cut.
- Podiatry (DPM) made the cut.
- Naturopathic Medicine (ND) in some interpretations remains eligible for higher limits due to accreditation nuance.
Physician Assistants—who manage complex internal medicine, staff emergency rooms, scrub into surgery, and serve as the primary providers for millions in rural America—did not.
The "Medical Model" argument died on the floor of the House. This proves that federal policy is no longer based on curriculum rigor, clinical responsibility, or patient safety. It is based on budgetary exposure. There are simply too many PAs and NPs graduating, and the government wants out of the business of funding them.
To PharmDs: Your "Professional" Status is Temporary
To my colleagues holding a Doctor of Pharmacy (PharmD): Do not get comfortable.
Right now, you are looking at the H.R. 1 student loan changes 2026 and breathing a sigh of relief. You are in Tier 1. You kept your $50,000 annual cap. You feel recognized. You feel like the government respects the "Dr." in front of your name.
You are misreading the room.
The exclusion of PAs is the "canary in the coal mine" for pharmacy. PAs practice diagnosis and prescribing—the very core of medicine. If the government can label them "non-professional," your title of "Doctor" is not the shield you think it is.
Why Pharmacists Are at Risk of Reclassification
Pharmacists face a high risk of future funding cuts because retail saturation and automation are devaluing the perceived complexity of the role in the eyes of policymakers. If the government’s goal is to cut spending, moving PharmDs to Tier 2 is the logical next step after defunding PAs and NPs.
Consider the optics. The Department of Education justified the Tier 2 caps by claiming they are "reining in inflated prices at graduate programs" where tuition has outpaced "modest earnings potential."
- Retail Saturation: The market is flooded. Wages in retail pharmacy have stagnated compared to inflation. If the Dept of Education looks at the ROI of a PharmD degree (high tuition, stagnating wages), it looks remarkably similar to the logic they used to cut Law Schools in previous drafts of legislation.
- Clinical vs. Retail: While clinical pharmacists are vital, the vast majority of the public—and the legislators—interact with pharmacists in a retail setting that they increasingly view as automated logistics rather than healthcare.
- The PA Precedent: PAs act as primary care providers and were still cut. If a provider who diagnoses and prescribes isn't "professional" enough for Tier 1 funding, how long until a provider who dispenses is cut too?
You are one budget reconciliation away from joining the "unprofessional" list.
A Quick Heads-Up for Clinicians Feeling the Squeeze
If reading about these cuts makes you worry about future staffing ratios—you’re right to be concerned.
In my analysis, these cuts will lead to a "brain drain" in primary care. Fewer graduates mean higher patient loads for those of us left. The "do more with less" era is escalating to "do everything with no one."
You cannot rely on the government to fix staffing. You have to rely on efficiency.
Rx Agent is your force multiplier. It helps you survive the increased workload by:
- Automating Clinical Research: Get evidence-based interaction checks and dosing guidelines in seconds.
- Navigating Regulation: Understand how policy changes like H.R. 1 impact your specific license and practice.
I joined the waitlist because I need to know if the regulatory landscape is shifting under my feet before the academic year starts.
👉 Get early access here: https://www.rxagent.co/
The Credentialing Trap: Doctorates on an Undergraduate Budget
For Physical Therapists (PTs), Occupational Therapists (OTs), and CRNAs, the situation is even more dire. We are witnessing the birth of the "Credentialing Trap."
What is the Credentialing Trap?
The Credentialing Trap occurs when employers and licensing boards demand doctoral-level degrees (DPT, OTD, DNP) for entry-level practice to increase professional prestige and competency, while federal loan policies fund students at undergraduate levels. This gap forces students to take out predatory private loans to meet the mandatory educational standards of their profession.
Let's look at the data for Allied Health:
- Physical Therapy: You cannot practice without a Doctorate of Physical Therapy (DPT).
- Nurse Anesthesiology: The CRNA entry-level degree is moving entirely to the doctorate (DNAP/DNP) by 2025/2026 mandates.
- The Funding: Under H.R. 1, these students are capped at $20,500 per year.
The Math of Exclusion
I have analyzed tuition costs for DPT programs. They routinely exceed $100,000 for the program.
- Scenario: A student enters DPT school with $30,000 in undergraduate debt.
- New Cap: H.R. 1 caps "Graduate" degrees at $100,000 aggregate lifetime limit.
- Result: The student can borrow $70,000 total for a degree that costs $110,000+.
- The Gap: They must find $40,000+ in private loans at 11-13% interest rates.
This is mathematically impossible for anyone without generational wealth. The result? Only the wealthy will become Physical Therapists. H.R. 1 has effectively privatized the cost of the allied health workforce while maintaining public control over their reimbursement rates (through Medicare cuts). It is a stranglehold that will choke the pipeline of new providers.
The Paradox of Project 2025: Direct Primary Care
One of the most ironic aspects of this legislation is how it contradicts the broader health goals of the conservative movement, specifically regarding Direct Primary Care (DPC).
The administration has championed DPC—a model where patients pay a monthly membership fee for access to a doctor, bypassing insurance—as the solution to healthcare costs. H.R. 1 even includes provisions allowing Health Savings Accounts (HSAs) to pay for DPC memberships, a massive demand stimulus.
But who staffs DPC clinics? To keep membership fees affordable ($50-$80/month), DPC practices rely heavily on Nurse Practitioners and PAs to handle routine acute care and follow-ups.
The Paradox:
- Stimulate Demand: The government uses tax breaks to encourage millions of Americans to join DPC clinics.
- Kill Supply: The government simultaneously makes it financially ruinous to become a PA or NP.
The result will be a DPC market that is flooded with patients but starved of providers, leading to rising membership fees that only the wealthy can afford. The populism of the policy is undermined by the austerity of the budget.
Workforce Implications: The Coming Exodus
The "Nursing labeled unprofessional degree" controversy is about more than hurt feelings; it is about workforce collapse.
140 lawmakers sent a letter warning that these caps will "make it significantly harder to finance graduate nursing degrees," specifically deterring students from underrepresented backgrounds.
1. Rural Health Collapse
Advanced Practice Registered Nurses (APRNs) and PAs are the backbone of rural health. They are the ones staffing the clinics in Mississippi, rural Oregon, and the Upper Peninsula of Michigan that physicians won't touch due to low reimbursement. When you force students to take private loans at 12% interest, they cannot afford to take a job in a rural clinic paying $95,000 a year. They must take the job in the affluent suburb paying $130,000 to service their debt. H.R. 1 essentially legislates a provider desert in rural America.
2. The Brain Drain
Experienced RNs looking to become NPs will look at the $20,500 cap, look at the tuition, and decide to stay at the bedside. Or, worse, they will leave healthcare entirely for industries that don't require taking on a mortgage-sized debt to advance.
3. The Liability Spike
For those who remain, patient ratios will skyrocket. The "do more with less" mantra of hospital administration will become "do everything with no one." New York Academy of Medicine President Ann Kurth put it best: "When one part of the health team is undermined, care for all is compromised."
Solution: Surviving the Squeeze with Rx Agent
We are entering an era of resource scarcity. Funding is being cut. Staffing is shrinking. Complexity is increasing.
If you are a PA, NP, or Pharmacist, you cannot rely on the government to bail you out. You cannot rely on more staffing. You have to rely on efficiency. The regulatory pressure is about to get worse. With fewer providers, the liability for those remaining increases. You need a force multiplier.
How can Rx Agent help clinicians during the workforce shortage?
Rx Agent acts as an AI-powered clinical force multiplier, providing instant answers to complex regulatory and clinical questions to reduce burnout. By automating the research process for guidelines and interactions, it allows overburdened providers to handle higher patient volumes safely.
This is where Rx Agent clinical AI becomes essential survival gear. You don't have time to dig through UpToDate for 15 minutes when you are covering the patient load of two providers. You don't have time to second-guess the new H.R. 1 repayment terms or the latest billing codes.
Rx Agent (rxagent.co) is built for the "unprofessional" professional.
- Instant Clinical Answers: Get evidence-based interaction checks and dosing guidelines in seconds.
- Regulatory Navigation: Understand how policy changes like H.R. 1 impact your specific license and practice.
- Liability Shield: Documentation assistance to protect your license when you are stretched thin.
The government has signaled that they do not value your education. They have capped your potential. Do not let them cap your efficiency.
The Final Word
Think of the healthcare system as a high-performance engine.
- The Doctors (MD/DO) are the pistons—essential, driving force.
- The Pharmacists are the fuel injectors—precise, critical.
- The PAs and NPs are the oil. We lubricate the system, fill the gaps, and keep the engine from overheating and seizing up.
H.R. 1 just decided that oil is a "non-professional" fluid. They’ve decided they can run the engine dry to save money on maintenance.
We all know what happens next. The engine seizes.
Don't be inside the vehicle when it does without an exit strategy. Secure your workflow with Rx Agent.
References
- Brusie, C. (2025, Dec 15). "Lawmakers Urge The DoED To Add Nursing To The List." Nurse.org.
- Nurse.org Staff. (2025). "140 Lawmakers Send Letter Urging DoED to Add Nursing To The List Of Professional Degrees."
- Nurse.org Staff. (2025). "The letter was sent by bipartisan leaders..."
- Mensik Kennedy, J. (2025). "ANA Statement." Nurse.org.
- Nurse.org Staff. (2025, Nov 26). "ED: 'Not a Value Judgment About Nurses'."
- Hess, C. (2025, Nov 21). "Nursing no longer considered a professional degree by Trump administration." Wisconsin Public Radio.
- Hess, C. (2025). "Students in programs that are designated as 'professional'..." WPR.
- Kurth, A. (2025). "Response to Stripping 'Professional Status'..." New York Academy of Medicine.
Frequently Asked Questions
About the Author
Dr. Zade Shammout, PharmD writes about prescription medications, pharmacy laws, and healthcare compliance for prescribers and pharmacists.